Perinatal Grief: Phases And Protocol

Coping with the loss of a loved one is always difficult, but what happens when that loss occurs during the course of the pregnancy? Today, we want to talk about perinatal grief. We find it necessary to make visible an issue that occurs more often than is believed and about which there is great misinformation.
In Spain, perinatal mortality designates the number of deaths produced between the 28th week of gestation until the first seven days of life for every 1,000 live and stillbirths. The neonatal mortality rate would be the number of deaths that occurred between birth and 28 days of life in a given year per 1,000 live births in that same year (González, Suárez, Polanco, Ledo and Rodríguez, 2013).
The WHO in the 10th revision of the International Classification of Diseases (ICD-10), differentiates the loss during pregnancy as follows:
- Early fetal death: refers to fetuses less than 22 weeks gestation and / or <500 grams of weight. It is known as “abortion.”
- Intermediate fetal death : includes fetuses between 22-28 weeks of gestation and / or weight between 500-999 grams.
- Late fetal death: includes fetal deaths from 1,000 grams of weight and / or greater than 28 completed weeks of gestation.

Authors, such as López (2011), extend the concept of mourning. It includes, like this:
- Cases of abortion (voluntary and involuntary).
- Voluntary interruption of pregnancy due to problems of the fetus or threat to the health of the mother.
- Selective reduction in multiple pregnancies.
- Intrapartum or intrauterine death.
- Loss in multiple and newborn pregnancies.
Loss during pregnancy has not always been of the same importance. Nowadays, thanks to the fact that there is more information and more sensitivity towards this event, protocols have been developed aimed at supporting parents during the grieving process.
Protocol for perinatal loss and grief
In the Guide for the Care of Perinatal and Neonatal Death, they mention some hospitals where these protocols are already being carried out. Two of these hospitals are:
- Donostia Hospital, in San Sebastián. Based on the initiative of a professional from the Maternity Service who requested the Basque Government’s Health Department to implement courses on perinatal bereavement aimed at professionals. The 33 midwives working in the service have received specific training on perinatal deaths.
- Basurto Hospital, in Bilbao. A Perinatal Grief Protocol has been developed in the Neonatology Unit. The contents are based on the rights of the child, actions directed at parents and those directed at the health team.
The protocol recommendations consist of providing care that reflects the parents’ natural desire to see and hug their child after birth, and provides useful tools to the professionals involved in caring for the process (Contreras, Ruiz, Orizaola and Odriozola , 2016).
These same authors distinguish different steps depending on the moment:
After communicating the news
- Establish a relationship with parents based on sensitivity.
- Understand the impact of the news on parents.
- Ensure that parents are accompanied throughout the process.
- Offer clear information about the different options they have. According to the association El Parto es Nuestro , when after performing certain medical tests it is discovered that the baby does not have a heartbeat, there are two possibilities. One would be expectant management, which consists of waiting for the body itself to naturally trigger the elimination of the remains. This process is very similar to that of childbirth. The second option would be curettage, necessary when the mother does not go into labor spontaneously.
During labor and delivery
If the parents have not raised any concerns about contact with their child, proceed as naturally and respectfully as you would with any parent who wishes to see the newborn.
After birth
- Guiding gently and individually while parents get to know their child.
- Normalize professional contact with the deceased child to show parents a way forward.
- Offer the possibility of having a memory of the baby.
- Respect and fully support the wishes of parents who decline to see or spend time with their child. Assess whether they want custody of a memory for some time. Assess whether they want the accompaniment to be carried out by another person.
Within this last section, it is important to note that article 40 of the Law of June 8, 1957 on the Civil Registry, according to the criteria of article 30 of the Civil Code, establishes that only those that survive 24 hours after complete detachment from the mother’s womb.
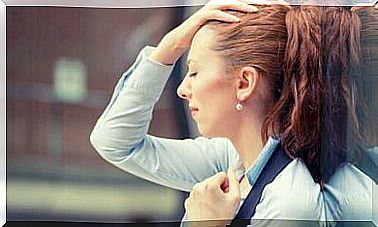
Coping and phases of perinatal grief
In the face of the loss of any loved one, especially in these cases, we must respect the freedom and the decisions made by the parents. You have to understand, listen and try to keep them as much control as possible over the development of events.
The phases that parents usually go through in these cases are three (López, 2011; cited in Vicente, 2014):
- First, shock and numbness, lightheadedness, and functional difficulty are experienced ; all accompanied by feelings of longing.
- Second, the disorientation and disorganization of everyday life. This goes hand in hand with the feeling of emptiness and helplessness.
- Finally, a reorganization is achieved in which life is rebuilt and the capacity for enjoyment is recovered, but without forgetting.
To face or cope with the death of the baby, there are, from different areas, resources and measures that support parents (Vicente, 2014):
Within the health field
- Referral and information on discharge resources. Offer couples and relatives information on bibliographic resources, web resources, associations, self-help groups, etc.
- Likewise, it is necessary to facilitate emotional expression in the absence of any type of judgment.
- Provide support during the hospitalization process, using listening as a therapeutic tool. Inform and guide to facilitate autonomous decision-making by parents.
- Likewise, it is necessary to train health personnel. Train skills and provide tools and techniques that improve care for perinatal grief and loss in the early stages.
Outside the health field
- Creation and development of information and social awareness campaigns.
- Creation and dynamization of Mutual Aid Groups : aimed at mothers and fathers, siblings, grandparents, etc.
- Support and accompaniment in the grieving process.
- Orientation in bureaucratic procedures.
- Counseling and grief therapy : at the couple, family or individual level.
In short, it is necessary to train professionals so that they can attend, accompany and support both parents and the family environment, without forgetting that it is the parents who must set the pace of the process.